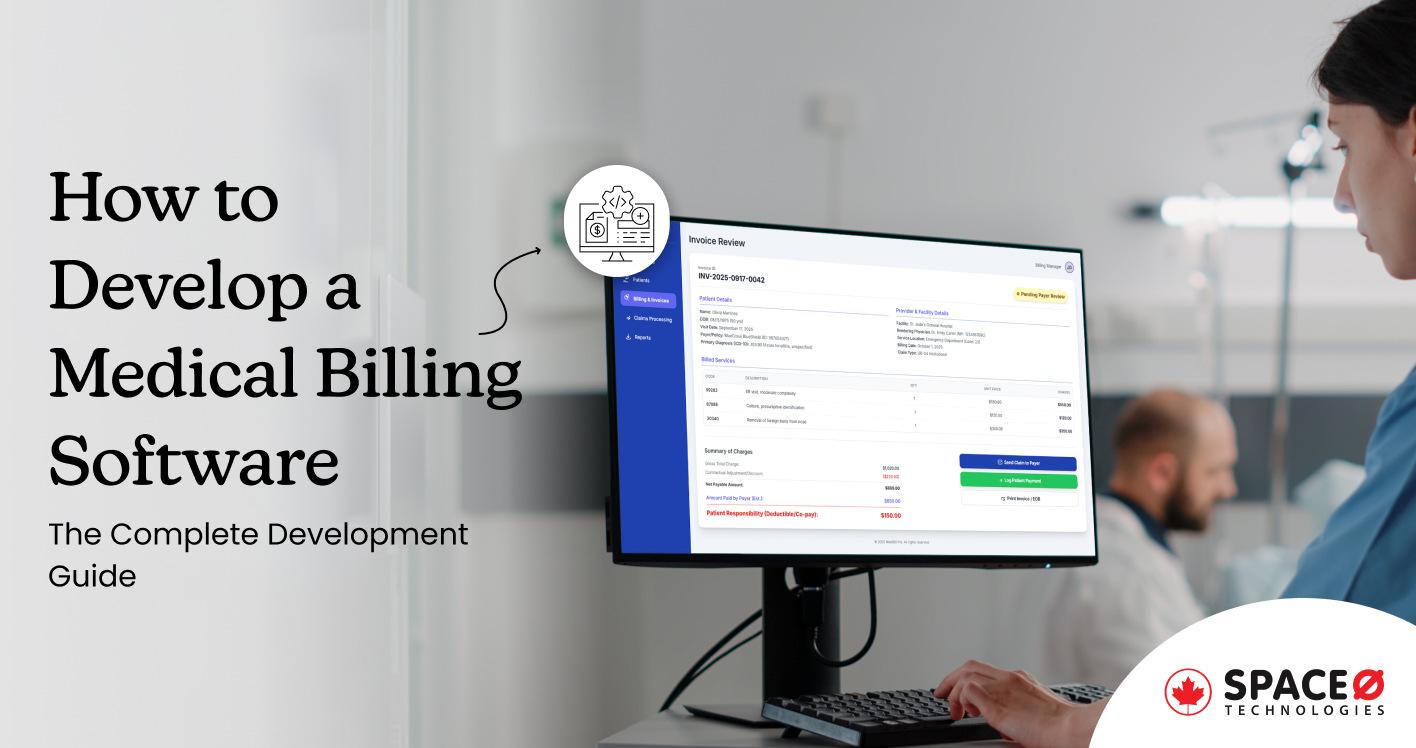
Medical Billing Software Development: The Complete Guide for Healthcare Providers
Your billing department just rejected another batch of claims. The insurance company says the codes are wrong. This happens in healthcare practices daily, and it’s costing you more than you realize.
Over 80% of medical bills contain errors, according to the beckershopsitalreview.com. That’s not a quality issue—it’s a systemic problem affecting your bottom line. Yet most healthcare organizations continue using decades-old billing approaches because they don’t know what’s possible with modern automated systems.
Here’s what they’re missing: Custom medical billing software that improves bill collections, reduces billing errors, and typically recovers their entire investment within 12 months.
Space-O Technologies, a healthcare and medical software development company, understands these challenges, and its team of experts has created a comprehensive guide that reveals:
- How medical billing software works
- Why custom solutions outperform off-the-shelf platforms
- What the development process looks like
- Realistic timelines and costs, and
- Critical success factors ensuring your investment delivers genuine ROI.
Whether you’re frustrated with your current billing process, planning to upgrade systems, or building from scratch, understanding medical billing software development helps you make informed decisions about the technology infrastructure that literally fuels your organization’s financial health.
What is Medical Billing Software?
Medical billing software is a digital system designed to automate and simplify the financial and administrative workflows of healthcare practices. It handles tasks like submitting insurance claims, processing patient payments, and managing invoices. By removing manual steps, it helps healthcare providers improve billing accuracy, cut down on errors, stay compliant with regulations, and strengthen overall revenue cycle performance.
Additionally, this type of healthcare and medical software allows you to capture clinical data, convert it to billable codes, verify insurance eligibility, submit claims electronically, track reimbursements in real-time, and generate comprehensive financial reports. For healthcare organizations struggling with claim denials, delayed payments, and data entry errors, implementing custom billing software transforms financial operations.Understanding the capabilities of billing software helps determine whether your organization needs a custom solution. Let’s explore why healthcare providers are shifting toward custom software development.
Example: A physiotherapy clinic sees 200+ patients each week. Before using billing software, the staff manually entered treatment notes, checked insurance coverage by phone, and submitted claims individually. Payments were delayed by 20–30 days because of coding errors and missing information.
With a custom medical billing system:
- Patient data is automatically synced from the EMR to the billing module.
- Eligibility checks run instantly, preventing services that won’t be reimbursed.
- Treatment notes are converted into accurate billing codes using predefined clinician templates.
- Claims are submitted electronically within minutes of the appointment.
- Denials are flagged automatically, including reasons and suggested corrections.
- The financial dashboard shows real-time revenue, pending claims, and aging reports.
As a result, the clinic reduced administrative workload, cut claim denials in half, and significantly improved cash flow—all by automating the billing cycle end to end.
Why Healthcare Providers Need Custom Billing Solutions
Healthcare organizations face three critical challenges that off-the-shelf solutions cannot adequately address:
- Financial impact: This report highlights that automated billing boosts transaction processing 28% while reducing administrative costs. A mid-size practice handling 500+ claims monthly could recover software investment within 12 months through improved collections alone.
- Compliance risk: Healthcare is the most regulated industry. For PIPEDA, violations can result in a CAD $100,000 fine per offense, as per a report from bakermckenzie. Custom solutions built with compliance from day one protect against catastrophic regulatory exposure.
- Scalability: Off-the-shelf software limits growth. Custom solutions scale with your practice, supporting multiple locations, departments, and increasing claim volumes without expensive migrations.
Now that you understand what billing software does, it’s crucial to recognize that not all billing solutions are created equal. The type of system you choose dramatically impacts implementation timeline, total cost of ownership, and long-term ROI.
Let’s examine the different approaches.
4 Types of Medical Billing Software to Develop
Choosing the right billing software type depends on your organization’s specific needs, budget, and long-term strategy. Here are the four main types of medical billing software that you can build based on your requirements:
1. Cloud-based billing software
Cloud-based systems are online platforms that let you manage invoices, payments, and claims from anywhere with an internet connection. The software provider hosts everything—no local servers required.
Pros:
- Scales effortlessly without costly hardware upgrades
- Accessible from any location with internet connection
- No local IT maintenance—vendor handles infrastructure and updates
- Lower upfront costs ($1,000–$3,000 monthly vs. $50,000+ for servers)
- Automatic security patches and compliance updates
- Built-in backup and disaster recovery
Cons:
- Requires stable internet connection (outages impact operations)
- Subscription model can mean higher long-term costs ($12,000–$60,000 annually)
- Less control over data location and security protocols
- Dependent on vendor’s uptime and reliability (99.9% SLAs typical)
Best for: Multi-location practices, organizations prioritizing cost efficiency and minimal IT overhead.
2. Standalone billing software
Standalone systems install directly on your servers or computers and operate independently, without an internet connection. The software manages billing only—no integration with other practice functions.
Pros:
- Advanced medical billing features optimized for specialized needs
- Complete control over data and software updates
- No reliance on the internet or external vendors
- One-time purchase cost with minimal ongoing fees
Cons:
- Not integrated with EHR, scheduling, or practice management systems (requires manual data entry)
- Requires dedicated local IT support and infrastructure maintenance
- No automatic updates—your team manages security patches
- Limited scalability across multiple locations
- Difficult to upgrade or switch systems later
Best for: Small practices with simple billing needs and dedicated IT resources; organizations needing offline capability.
3. Integrated medical billing software
Integrated systems combine billing, appointment scheduling, electronic health records, patient management, and practice operations into a single unified platform.
Pros:
- All-in-one solution eliminating the need for multiple systems
- Automatic data flow between clinical and billing functions (reduces manual entry errors by 60-70%)
- Unified patient information accessible across departments
- Streamlined workflows and simplified staff training
- Better data consistency and fewer billing errors
Cons:
- Complex to develop, implement, and learn (requires comprehensive training)
- More expensive upfront ($120,000–$250,000 custom development)
- Switching platforms later is complex and disruptive
- Over-engineered if you only need billing (paying for features you don’t use)
- Longer implementation timelines (6–18 months)
Best for: Multi-department practices, hospitals, healthcare systems seeking unified operations; organizations building new systems from scratch.
4. Customized billing software solutions
Custom billing software for medical institutes is built specifically for your organization’s unique workflows, requirements, and processes. Rather than forcing your practice to fit software, software adapts to your practice.
Pros:
- Perfectly matches your specific workflows and processes
- Unlimited customization—no vendor limitations
- Integrates deeply with your existing systems (legacy or modern)
- Scalable as your organization grows (no costly migrations)
- You own the code and avoid vendor lock-in
- Lower long-term costs (no licensing fees)
- Better long-term ROI (especially over 5+ years)
Cons:
- Higher upfront development cost ($80,000–$250,000+)
- Longer initial development timeline (3–18 months)
- Requires experienced healthcare software developers
- Ongoing maintenance responsibility (15-20% of development cost annually)
Best for: Complex practices with unique requirements; healthcare systems with specific workflows; organizations planning long-term use (5+ years).
Confused About Billing Software? Don’t Pick the Wrong One
Let Space-O analyze your practice needs and suggest the perfect solution—no guesswork, no overwhelm.
Understanding which billing software type fits your organization is essential, but knowing exactly what features that software must include is equally critical. The difference between adequate and exceptional billing systems often comes down to whether they include the right capabilities.
Let’s explore the essential medical billing software features every billing system must deliver.
7 Essential Features Every Medical Billing Software Must Have
Medical billing software offers a wide range of capabilities. But, for developing a MVP (Minimum Viable Product) or planning your software project, you need to learn about essential features that directly impact revenue and efficiency:
1. Billing automation
Billing automation streamlines the entire invoicing workflow so medical teams can spend more time on patient care and less on administrative tasks. Once a patient is registered, the system carries their information through every step—claim submission, verification, and reimbursement—without requiring constant manual input.
You simply configure the billing rules once. After that, the software automatically applies the correct medical codes, charges, and procedures for each patient. This not only reduces errors but also eliminates repetitive data entry, making the billing process faster, cleaner, and far more efficient
2. Electronic Health Records (EHR) integration
EHR software development and integrations enable seamless data flow between clinical documentation and billing systems and prevent manual re-entry of patient information.
When clinicians document procedures in the EHR, the billing system automatically captures and converts that data to billable codes. Uses healthcare data standards (HL7, FHIR), ensuring compatibility with Epic, Cerner, Athena, and other major EHR platforms.
3. Customizable interface
Medical billing software must be intuitive – billing staff use it 6-8 hours daily. The best systems offer minimal clicks for everyday tasks, clear visual hierarchy, mobile responsiveness, customizable dashboards, and WCAG 2.1 AA accessibility compliance.
Systems that allow customization of invoicing workflows achieve higher adoption rates than rigid, one-size-fits-all platforms.
4. Reporting and analytics capabilities
Integrating a reporting and analytics dashboard turns your billing data into clear insights you can actually use. You get essential reports such as Days Sales Outstanding (DSO), denial trends, revenue by service, provider, or payer, aging summaries, and cash flow forecasts.
With advanced analytics, you can spot what’s slowing down your billing operations and uncover deeper issues you might otherwise miss. Many healthcare organizations that adopt analytics see DSO drop by 10–15 days, resulting in more than $500,000 in annual savings for larger practices.
5. Patient portal and communication
Adding a patient portal and dashboard lowers your administrative workload and makes the billing experience smoother for patients. With a portal, patients can easily view their bills, make payments online, and contact billing staff without calling the clinic.
This leads to fewer billing-related inquiries, quicker payments thanks to online options, higher patient satisfaction, and the ability to offer flexible payment plans.
6. Insurance eligibility verification
Real-time insurance eligibility verification, powered by modern insurance software development, ensures providers instantly confirm a patient’s coverage, deductibles, and prior authorization requirements before delivering care.
This is crucial because eligibility issues are the #1 cause of claim denials, leading to delayed payments and lost revenue. By automating these checks, healthcare organizations reduce coverage-related denials, improve billing accuracy, and prevent preventable revenue leakage, ensuring every claim starts on the right track.
7. Compliance and security
Compliance and security are essential features in any healthcare or insurance software development project because they protect sensitive patient and financial data from breaches and regulatory violations.
This feature ensures the system adheres to strict standards such as PIPEDA and HIPAA by using tools like end-to-end encryption, role-based access controls, MFA, and penetration testing.
Pro tip: When developing your MVP, prioritize automation, EHR integration, and compliance—these directly impact revenue and organizational risk. Add analytics, patient portals, and customization in Phase 2 based on user feedback and organizational needs.
Now that you understand the essential features billing software must deliver, the question becomes: how do you actually build this system? Understanding the software development process helps you plan realistic timelines, budgets, and resource requirements.
Let’s walk through each phase of building medical billing software.
How to Build Medical Billing Software: 8-Phase Development Roadmap
Building medical billing software requires methodical planning, specialized technical expertise, and an understanding of healthcare operations. Here’s how successful organizations approach development:
Phase 1: Requirements definition and market research
During this phase, the focus is on gathering accurate, detailed requirements that define how the medical billing software should function. The process typically involves:
- Stakeholder collaboration: Engaging healthcare providers, billing staff, physicians, and administrators to uncover workflow issues, compliance needs, and daily operational challenges.
- Workflow and pain-point analysis: Identifying bottlenecks, manual tasks, and areas where automation can improve accuracy and efficiency.
- Market and competitor research: Studying existing solutions to identify gaps, opportunities, and features that can give your software a competitive edge.
- Defining the product foundation: Documenting the project vision, core objectives, scope, success metrics, and realistic development timelines.
This groundwork ensures the development process begins with complete clarity, reducing the chances of misalignment and costly rework.
Space-O Technologies supports this phase by assigning skilled analysts and domain experts to convert these findings into a structured and comprehensive SRS document. Creating a software requirement specifications helps you to establish a strong foundation for accurate and efficient development.
Phase 2: Proof of Concept (PoC) and MVP strategy
This phase focuses on validating ideas before committing to full-scale development:
- Proof of concept (PoC): Test core features and confirm technical feasibility before building the full product.
- MVP development: Build a minimum viable product focusing on essential functionalities such as automated billing, eligibility verification, and basic claims processing.
- Early user launch: Release the MVP to real users to gather feedback and validate market fit.
- Feature refinement: Use user insights to improve features, optimize workflows, and ensure the product addresses real-world needs.
- Cost and time efficiency: Accelerate time-to-market while minimizing initial development costs and reducing the risk of costly rework.
Space-O Technologies supports this phase with custom MVP development services, helping teams validate assumptions, reduce risks, and move into full development with confidence.
Phase 3: Technical architecture and technology stack
In this phase, the focus is on designing a robust, scalable, and secure foundation for medical billing software. The technical architecture defines how different system components—such as user interfaces, databases, APIs, and insurance integrations—work together.
Selecting the right technology stack ensures the software can efficiently handle real-time billing, eligibility verification, claims processing, and reporting while maintaining compliance and security. Here’s a table showing a typical technology stack for medical billing software development:
| Key Activity | Recommended Technology Stack | Purpose / Notes |
|---|---|---|
| Programming languages | Java, C#, Python, or Node.js | Core logic and backend development |
| Frameworks | Spring Boot, .NET Core, Django, Express.js | Speeds up development and enforces structured coding practices |
| Databases | PostgreSQL, MySQL, MongoDB, Microsoft SQL Server | Store patient records, billing data, claims, and transaction logs |
| Cloud services | AWS, Microsoft Azure, Google Cloud | Scalability, high availability, and secure hosting |
| Frontend | React, Angular, Vue.js | Interactive user interfaces for billing staff and healthcare providers |
| APIs / Integration tools | RESTful APIs, HL7, FHIR, SOAP | Connect with EHR systems, insurance providers, and payment gateways |
At Space-O Technologies, we guide this phase by leveraging our expertise in healthcare software development. Our team designs the technical architecture and selects the optimal and modern technology stack to create a secure, compliant, and high-performance solution.
Phase 4: Design and user experience development
This phase focuses on creating an intuitive, efficient, and user-friendly interface for medical billing software. The goal is to ensure that the software aligns with real-world healthcare workflows and is easy for billing staff and administrators to navigate, even during extended daily use.
Key activities include:
- Wireframes and mockups: Develop visual blueprints for screens, workflows, and user interactions.
- Interactive prototypes: Build clickable versions of the software to test flow, navigation, and feature placement before development.
- Usability testing: Engage real billing staff and healthcare providers to evaluate interface intuitiveness, identify pain points, and gather actionable feedback.
- User-centered design: Balance professional functionality with simplicity, ensuring staff can perform billing tasks efficiently without confusion or delays.
- Iterative refinement: Continuously refine designs based on testing insights to improve user adoption, satisfaction, and overall productivity.
At Space-O Technologies, we focus on the process of crafting software designs that reflect real healthcare workflows. Our team creates wireframes, prototypes, and user-tested interfaces to ensure the software is not only functional but also intuitive, helping billing staff work efficiently, reduce errors, and increase adoption rates.
Phase 5: Agile software development
This phase focuses on building the medical billing software iteratively and flexibly to ensure alignment with requirements and reduce development risks. Agile methodology breaks development into short sprints (typically 2-week cycles), guided by the principles of the Agile Manifesto. It allows continuous stakeholder feedback and faster course corrections.
Key development activities include:
- Backend development: Implement server-side logic, database connections, APIs, and integrations with EHR systems and insurance providers.
- Frontend development: Build intuitive, accessible user interfaces that comply with usability standards for daily billing workflows.
- Security implementation: Integrate HIPAA-compliant measures, encryption, authentication, and access controls to protect sensitive data.
- Sprint planning and reviews: Conduct regular sprint meetings and reviews to track progress, gather stakeholder feedback, and adjust priorities as needed.
- Resource management: Mid-range systems typically involve 4–6 experienced developers working over 6–9 months to deliver a robust, scalable solution.
At Space-O Technologies, we follow agile software development practices to ensure each iteration reflects real user needs. Our teams implement backend infrastructure, APIs, EHR integrations, and secure, accessible frontends while continuously incorporating feedback, reducing costly mistakes.
Phase 6: Testing and quality Assurance
This phase focuses on ensuring the medical billing software is reliable, secure, and performs as expected under all conditions. Rigorous testing identifies and resolves issues before the software reaches end-users, reducing errors, downtime, and costly rework.
Here are the different types of software testing to perform before launch:
- Functional testing: Verify that every feature meets specifications and user requirements.
- Regression testing: Ensure updates or new features do not break existing functionality.
- Performance testing: Evaluate system behavior under peak loads to ensure stability and speed.
- Security testing: Identify vulnerabilities and verify encryption, authentication, and access controls.
- Integration testing: Confirm smooth connectivity with EHR systems, insurance providers, and payment gateways.
- Manual and automated testing: Manual testing captures usability and user experience issues, while automated testing efficiently verifies performance, security, and repetitive tasks.
- QA planning: Allocate sufficient development time and resources for thorough testing to prevent production issues.
At Space-O Technologies, we implement a software testing life cycle and quality assurance process that combines manual and automated testing, ensuring the software is fully functional, secure, and ready for real-world use.
Phase 7: Deployment and user training
This phase ensures a smooth transition from development to real-world use, minimizing disruption and maximizing adoption across the organization.
Key activities include:
- Phased rollout: Deploy the software department by department, rather than converting the entire organization at once, to reduce risk and ensure manageable adoption.
- User training: Conduct comprehensive sessions for billing staff, administrators, and healthcare providers, covering key features, workflows, troubleshooting, and best practices.
- Documentation: Provide detailed manuals, guides, and resources to support users during the transition.
- Parallel running: Initially operate the new system alongside legacy systems to provide a safety net, ensuring no disruption to billing or claims processing.
- Ongoing support: Offer continuous assistance during the adoption period to address user questions, refine processes, and ensure smooth operation.
We manage deployment using top software development tools and combine phased rollout, hands-on user training to ensure organizations adopt the new medical billing software efficiently. Our approach minimizes downtime, boosts user confidence, and accelerates full operational integration.
Phase 8: Maintenance and continuous improvement
Provide monthly security patches, quarterly compliance updates, and annual coding library updates. Monitor performance, address user feedback, and develop new features addressing emerging needs. Ongoing maintenance costs of initial software development annually—critical to long-term software viability.
Now that you understand the development process, the critical question becomes: how long will this actually take, and what’s the real cost? Timeline and budget planning determine whether your project stays on track or faces delays and cost overruns. The top healthcare software development companies, like Space-O Technologies, help you provide realistic cost and complexity.
Let’s break down realistic budget expectations based on complexity.
Medical Billing Software Development Cost: Realistic Pricing By Complexity
The cost of developing custom medical billing software ranges from $30,000 for a basic application to over $300,000 for an advanced, enterprise-grade system. Off-the-shelf solutions are available as subscription services, generally costing between $50 and $599+ per provider per month.
| Solution Type | Cost Range | Best For |
|---|---|---|
| Basic Custom | $30K–$100K | Small clinics with simple billing |
| Mid-Range Custom | $55K–$150K | Growing practices with EHR integration |
| Enterprise Custom | $150K–$350K+ | Large systems, multi-location, AI analytics |
| Off-the-Shelf | $50–$599/provider/month | Practices wanting quick deployment |
Factors affecting the cost of medical billing software development
- Feature complexity: Advanced features like AI analytics, telemedicine integration, and complex reporting capabilities add $10K–$50K each to development costs. Basic systems with just patient registration and claims processing cost significantly less than feature-rich platforms.
- System integrations: Connecting with EHR systems (Epic, Cerner, Athena), practice management platforms, and insurance databases adds $15K–$50K per integration. Legacy system integrations requiring custom middleware cost substantially more.
- Compliance and security: Implementing HIPAA requirements, encryption, access controls, and audit trails adds 15-25% ($20K–$60K) to total project costs. Regular penetration testing and security certification increase compliance expenses.
- Development team location: US-based developers charge $100–$200/hour, while offshore developers cost $25–$50/hour. However, offshore development may require additional oversight and investment in communication.
- Platform selection: Web-based applications cost less than developing native iOS and Android mobile apps. Mobile development adds $20K–$80K to total project costs.
Now that you understand healthcare software development costs, you can see that they present unique challenges that require mitigation strategies. Let’s explore the obstacles you’ll face.
Your Billing Software Might Be Costing You Thousands.
Build a custom medical billing system with Space-O that reduces errors, speeds claims, and improves cash flow.
Key Challenges of Medical Billing Software Development ( + How to Overcome Them)
Building healthcare software is different—it comes with challenges that typical software projects never face. The good news? These software development challenges are completely manageable if you know what’s coming. Understanding them upfront lets you plan accordingly and avoid costly mistakes.
1. Data security and privacy
The challenge: Healthcare is the #1 target for cyberattacks. Patient data breaches cost healthcare organizations $10.93 million on average, according to the report from IBM. That’s before fines from regulatory bodies or the hit to your reputation.
The solution: Don’t leave security as an afterthought—build it in from the start. Implement AES-256 encryption for stored data, TLS 1.3 for data in transit, role-based access controls, comprehensive audit logging, and penetration testing before launch. Hire security experts during the architecture phase. Retrofitting security later costs 3-5x more and often leaves gaps.
2. Regulatory complexity
The challenge: Healthcare regulations never stop changing. ICD-10 codes update every October 1st. HIPAA requirements, state regulations, and insurance company rules are constantly changing. Non-compliance doesn’t just mean fines; it can result in practice suspension.
The solution: Make compliance part of your system’s DNA, not an add-on. Engage compliance experts during the requirements phase so you understand what you’re building toward. Then monitor regulatory changes quarterly. Document everything meticulously for audits.
3. System integration
The challenge: Most healthcare organizations juggle 10-15+ systems simultaneously—EHR platforms, accounting software, insurance systems, you name it. Legacy systems often lack modern APIs, meaning you need custom middleware just to make them talk. Each integration costs $15K–$50K and adds 2-4 weeks to your timeline.
The solution: Map out every integration you need during discovery—don’t discover this halfway through development. Budget for middleware development upfront. Build robust error-handling and data-reconciliation processes so that when systems do talk to each other, data remains accurate. Test integrations thoroughly before going live.
4. Performance at scale
The challenge: Your system needs to handle hundreds to thousands of claims daily without slowing down. Here’s the kicker: Most healthcare billing system failures occur during peak-volume periods, such as month-end submissions. That’s when you need it most.
The solution: Load test your system before launch using realistic claim volumes and real peak-period scenarios. Optimize your database and implement caching to reduce database queries. Use a cloud infrastructure that auto-scales during busy periods. Plan your infrastructure for 3-5x your current volume—this prevents expensive rebuilds as you grow.
Now that you understand the challenges you can expect, the next critical decision is your technology foundation. The tools and platforms you choose are backend frameworks, databases, and infrastructure, which directly impact reliability, security, scalability, and your ability to grow.
Let’s explore which technology decisions actually matter.
Healthcare Compliance Requirements: HIPAA, PIPEDA, and Beyond
Regulatory bodies take data protection seriously, and non-compliance carries severe penalties including fines, practice suspension, and reputation damage. Whether you’re building for the USA, Canada, or multi-regional healthcare organizations, understanding these requirements in your system from day one is non-negotiable.
Here’s what you need to know for each region.
- HIPAA (United States): Administrative safeguards (policies, training), physical safeguards (facility security), technical safeguards (encryption, access controls, audit logs). Documentation must be comprehensive and ready for regulatory inspection.
- PIPEDA (Canada): Personal Information Protection and Electronic Documents Act governs patient data privacy. Requires consent for data collection, secure data handling, and breach notification within 30 days. Canadian healthcare organizations must comply with provincial health information privacy laws in addition to PIPEDA.
- Provincial Health Privacy Laws (Canada): Each province has specific regulations. Ontario: Health Information Protection Act (HIPAA). British Columbia: Personal Information Protection Act. Alberta: Health Information Act. These often impose stricter requirements than HIPAA.
Additional requirements: GDPR (if serving EU patients), state-specific regulations, insurance company requirements, and facility-type-specific compliance. Understanding compliance requirements and implementing them correctly is essential, but even the best technical implementation fails without proven best practices. For the error-free implementation, outsourcing healthcare software development services can be a small decision to follow established implementation patterns and consistently achieve better outcomes.
Build a Medical Billing Software With Space-O Technologies
Space-O Technologies specializes in developing custom medical billing software for healthcare organizations. Over the years, we’ve delivered healthcare software solutions for many organizations, consistently achieving significant improvements in collections velocity, error reduction, and operational efficiency.
Our expertise includes:
- HIPAA and PIPEDA-compliant architecture (zero compliance violations across our projects)
- EHR/PM system integrations (Epic, Cerner, Athena, and legacy systems)
- Revenue cycle automation and optimization
- Enterprise-scale solutions for clinics through multi-facility healthcare systems
- Ongoing maintenance and support, ensuring long-term success
Why choose Space-O Technologies:
- 300+ successful software projects delivered
- Proven track record
- Dedicated healthcare software expertise and compliance knowledge
- Full-service development from discovery through post-launch maintenance
- Transparent pricing and realistic timelines
Ready to transform your billing operations? Let’s build custom medical billing software tailored to your organization’s unique requirements.
Build Your Medical Billing Software With Expert Guidance
Turn your medical billing idea into a secure, compliant, and scalable solution—built by experienced developers of our software development company.
Frequently Asked Questions: Medical Billing Software Development
How long does it typically take for billing staff to adopt new medical billing software?
Billing staff become proficient within 2-4 weeks with proper training and support. However, full organizational productivity (matching pre-implementation speeds) usually takes 2-3 months as staff build confidence and encounter real-world scenarios.
Can existing medical billing systems be migrated to custom software without losing historical data?
Absolutely. Most healthcare organizations move from outdated billing platforms to custom-built medical billing software without losing any patient, claims, or financial data. A successful migration depends on a structured process that ensures every piece of information is extracted, cleaned, validated, and imported securely.
How it works:
- Data extraction from the old system: Your development team pulls patient records, claims history, ledgers, insurance details, CPT/ICD codes, audit logs, and any other billing datasets.
- Data cleaning & mapping: Duplicate, inconsistent, or incomplete records are fixed. Every field is mapped to the correct structure in your new custom system.
- Secure data transfer: Encrypted transfer methods ensure PHI protection and compliance with HIPAA, PIPEDA, and industry standards.
- Validation & testing: Developers run multiple rounds of verification to confirm that imported data matches the original system exactly—no missing claims, no lost billing history.
- Incremental cutover: Many teams migrate the bulk data first, then sync recent updates to ensure a smooth transition without downtime.
What tech stack is needed for medical billing and coding?
Building medical billing software requires a reliable, scalable tech stack that connects the frontend, backend, database, mobile apps, cloud infrastructure, and all third-party integrations used for claims, clearinghouses, and EHR systems. Below is a commonly used, production-ready stack:
- Backend: Node.js with Nest.js or Express.js, TypeScript, REST/GraphQL APIs, microservices architecture.
- Frontend: JavaScript, TypeScript, HTML5, CSS, React or Next.js (with Redux or MobX), Cypress, Storybook, Jest.
- iOS App: Swift, RxSwift, MVVM or Redux architecture, XCTest, SnapshotTesting.
- Android App: Kotlin, Coroutines or RxJava, Dagger/Hilt, Retrofit, Room, Clean Architecture.
- Cloud & Infrastructure: AWS or Google Cloud (ECS/Lambda, API Gateway, RDS/Firestore, S3/Cloud Storage, IAM), Docker, CI/CD pipelines.
Can the new system integrate with EHR/EMR platforms?
Yes. Modern medical billing systems commonly integrate with EHR/EMR systems via HL7/FHIR APIs to synchronize patient records, claims, and schedules in real time.
Will staff need training to use the new software?
Most custom solutions include onboarding, documentation, role-based tutorials, and admin training to ensure smooth adoption and reduce workflow disruption.
How secure is the data stored in the new billing system?
A secure system uses end-to-end encryption, role-based access, multi-factor authentication, regular security audits, and cloud infrastructure that meets healthcare compliance requirements.
All our projects are secured by NDA
100% Secure. Zero Spam
*All your data will remain strictly confidential.
Trusted by


Bashar Anabtawi
Canada
“I was mostly happy with the high level of experience and professionalism of the various teams that worked on my project. Not only they clearly understood my exact technical requirements but even suggested better ways in doing them. The Communication tools that were used were excellent and easy. And finally and most importantly, the interaction, follow up and support from the top management was great. Space-O not delivered a high quality product but exceeded my expectations! I would definitely hire them again for future jobs!”

Canada Office
2 County Court Blvd., Suite 400,
Brampton, Ontario L6W 3W8
Phone: +1 (602) 737-0187
Email: sales@spaceo.ca

